Antimicrobial resistance to Helicobacter pylori or H. Pylori can slow down the rate at which H. Pylori bacteria can be eradicated. Antimicrobial resistance is when bacteria develop resistance towards antibiotics, nullifying the effects of a drug. To detect H. Pylori drug resistance in the country, a device is being used at the national referral hospital. H. Pylori is a bacteria known to be a major risk factor for stomach cancer.
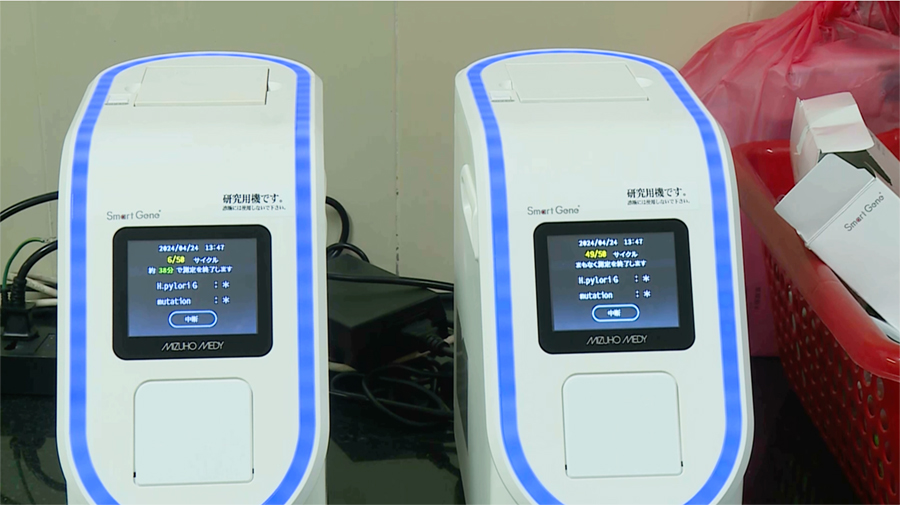
The device takes the gastric juice of a person during endoscopy. The results, which shows the status of H. Pylori and antimicrobial resistance to H. Pylori will be ready within 15 to 40 minutes.
Last month alone, about 70 people took the test and more than 20 per cent of them were found to have resistance to H. Pylori antibiotics.
The device was provided to the national referral hospital as part of the Science and Technology Research Partnership for Sustainable Development project, which is supported by JICA.
“We try to implement two of the tools for eradicating gastric cancer in Bhutan. One is the stool antigen test kit. That gives 15 minutes of the result of the Helicobacter pylori using your stool samples. The other one is the gene-based device, that can be used for asymptomatic patients who have the ulcer and severe gastritis,” said Takashi Matsumoto, Professor at Japan Agency for Medical Research and Development.
Doctors from the national referral hospital say the hospital usually detects antibiotics’ resistance to H. Pylori by providing medicines and checking its effectiveness.
Doctors added that people detected with H. Pylori are given triple therapy by providing clarithromycin, amoxicillin, and pantoprazole antibiotics. They are re-evaluated after three months.
If the person tests positive again, a person is treated with quadruple therapy with tetracycline, tinidazole, pantoprazole and bismuth antibiotics for two weeks and re-evaluated after another three months.
“Usually, we call them after three months and do either stool check-up or sometimes we do a biopsy, which is also depending on the individual patient. And if infection is still persisting, there can be two reasons; one is probably the antibiotic is not working. Second, is probably the patient’s compliance is not there, the patient is not taking medicine on time, and they have not completed the treatment. So, these two factors can lead to persistent infection,” said Dr Prabhat Pradhan, Oncosurgeon at national referral hospital.
However, he added that the patients do not come for the follow-ups. He said they only visit the hospital when the case become severe.
Eradication of H. Pylori is one of the strategic actions to prevent and reduce gastric cancer cases and deaths.
During the recent Gastric Cancer Flagship Programme, over 100,000 individuals were detected with H Pylori through screening campaigns.
As a follow-up to the flagship programme, the health ministry is currently developing a sustainable way to solve gastric cancer-related issues including H Pylori.
“We are developing a strategy where the screening will be looked into in the routine services meaning it will be incorporated into the routine services, while we continue to follow up on those that are positive, that have been detected with H. Pylori,” said Laigden Dzed, Chief Programme Officer of Non-Communicable Disease Division.
He added the ministry will also provide necessary services such as endoscopy and surgeries.
According to the recent health flagship report, the prevalence rate of H. Pylori is 66-82 per cent in the country.
Singye Dema
Edited by Tshering Zam